Pain after a cesarean section most commonly originates in the muscles and the nerves. Actually, aches and pains in the muscles are the most common source of chronic pain in the body. Both natural and traumatic events might bring on muscle soreness (like surgery or childbirth).
Many of the components for a chronic pain condition are present in the hormonal changes of pregnancy and delivery, as well as the lack of sleep and the stress of caring for a newborn.
Myofascial pain syndrome (MPS) is the medical term for this condition. MPS occurs when a muscle (for whatever cause) tenses and contracts excessively, generating tight bands (have you ever felt a knot of muscle in your neck? That’s the kind of tight band or knot that happens with MPS, only with MPS, the knot won’t go away). Because they restrict blood flow and squeeze nerves, spasms are incredibly painful.
In the aftermath of a cesarean section, this myofascial pain condition might manifest in the abdominal wall or the pelvic floor muscles (those are the muscles that you squeeze to stop your flow of urine and the muscles that contract during orgasm).

Is it a Muscle Pain?
Muscle pain can be excruciating and is typically (but not always) exacerbated by movement (including sex). A common analogy I’ve heard is that it feels like “a bowling ball” or “fist in the vagina.” The phrase “my insides are coming out” also comes to mind. Some female patients describe it as a cramping or squeezing sensation.
Since each person feels pain differently, there is a wide range in how it is described. Pelvic floor muscles protect the bowel and bladder from Pain during or after bowel movements, a frequent need to urinate, and urgency is all possible side effects of MPS.
Muscle discomfort and MPS are diagnosed clinically because there are no reliable diagnostic tests available. Pain in the abdominal region or the pelvic floor may be misdiagnosed by someone who isn’t trained to do so.
However, if the pain increases when you lie on your back, press on your stomach, and raise your head off the bed, the abdominal wall is likely the source (lifting your head flexes the belly muscles, and worsens of pain while the muscles are working can be a sign of MPS). Your doctor should also check for trigger points and other knots in the muscle using touch.
A pelvic exam is needed to diagnose pelvic floor MPS. Tight bands of muscle (like a violin string) can be felt by the examiner, and stroking them causes the same pain. Many women report that their partners feel like they are striking “a wall or blockage” when they come into contact with these tight bands of muscle during sexual activity.
Selecting Preferred Treatment
Once MPS is identified, most female patients react favorably to treatment. Visit a physical therapist who specializes in pelvic floor issues. A member of the International Pelvic Pain Society can be located at (enter your country, state, and city and a list of providers will appear, you will be able to tell who is a physical therapist and who is not).
Physical therapists use manual therapy to relax muscle knots and spasms (they may do other kinds of treatments as well). The following are examples of other treatment options:
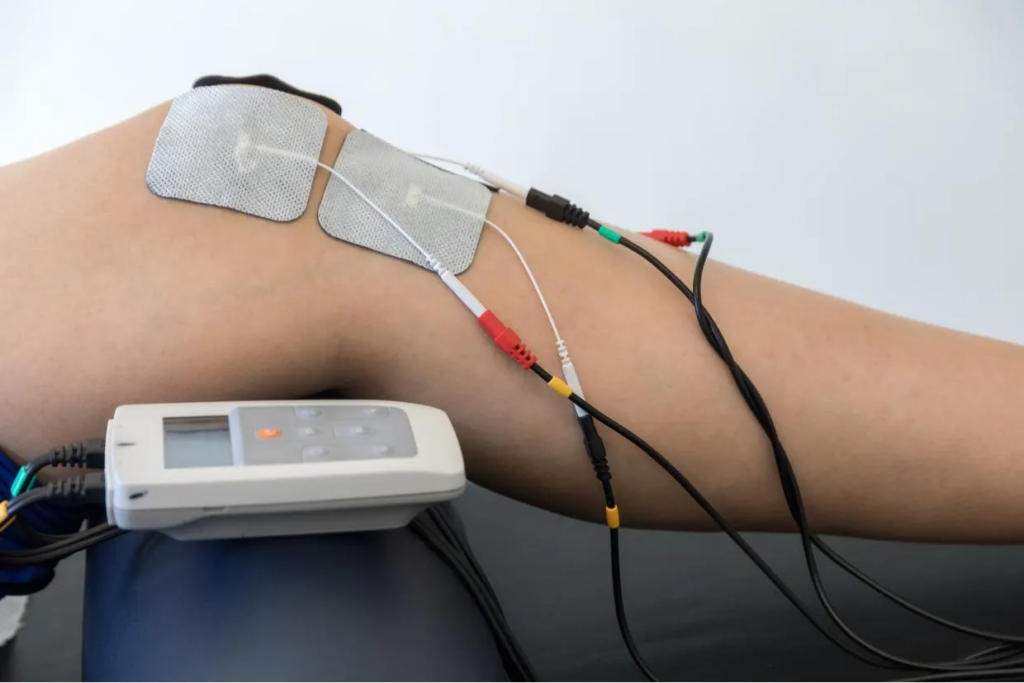
TENS Unit/Machine
A compact tool for stimulating abdominal muscles with electric current. A physiotherapist should set this up for you (there are specific settings). Pain in the abdominal wall may respond well to a transcutaneous electrical nerve stimulation device (TENS).
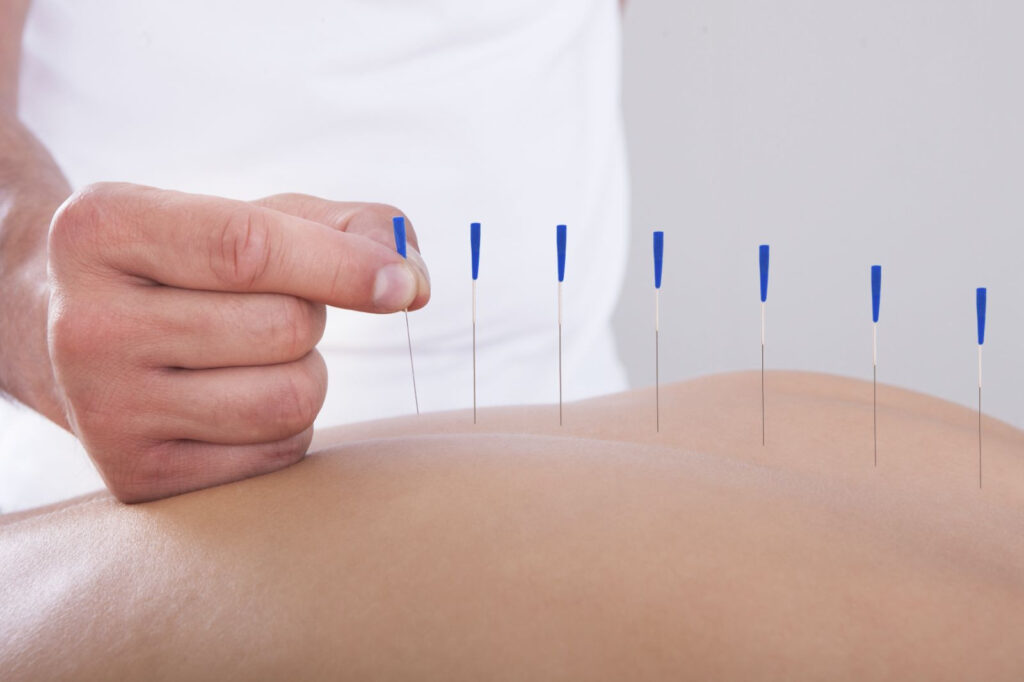
Injections at Trigger Points
Needles are used to manually break apart muscular bands and knots. This is made more bearable with the help of a little local anesthetic (it sounds worse than it is). Injections into trigger points are helpful, but they should be used in conjunction with physical therapy and ibuprofen or another anti-inflammatory medication.
A course of prescription dosage ibuprofen every 8 hours for 10-14 days may help reduce inflammation and stop the cycle of pain if there are no contraindications.
Drugs for Nerve Pain
Chronic pain can worsen as a result of altered nerve system signaling after a period of several months (think of it as the volume being turned up too loud in the nervous system). Medications for nerve pain, such as nortriptyline or gabapentin, can slow or stop these developments. There is no requirement for the drugs to be taken forever. Reducing pain often speeds up the neurological system’s recovery, allowing patients to wean off their drugs. It is acceptable to use nortriptyline during nursing.
Injections of Botox
That’s right, you spotted a typo. Whenever conventional methods of alleviating muscle spasms, such as physical therapy, have failed, Botox injections can be used to effectively stop the spasm cycle.
They have to be used in conjunction with physical therapy and only last for around 12 weeks. In order to ensure that the effects of the physical therapy continue long after the spasm cycle has been broken, the therapist will work with you to retrain your muscles. You shouldn’t have Botox if you’re nursing.
Getting Slimmer is the Goal
Muscle pain is exacerbated by the mechanical stress of carrying around more weight, which is common after giving birth. And because it stores excess energy as fat, more weight around the middle can also increase the production of inflammatory chemicals that contribute to the discomfort experienced.
Sport or Other Forms of Physical Exertion
Muscles are designed to be worked, even if doing so causes discomfort. If you stop using them, the blood stops flowing to them, and the agony gets greater. When you don’t use your muscles, they shrink.
Walking in a pool (the water helps to lift your body weight, putting less tension on the muscles), walking around the block, and gentle yoga classes are all great ways to get into an exercise routine. It’s best to ease into a fitness routine by doing so every other day at first to give muscles time to recover.
Constipation Management
When you strain, you overwork the muscles in your pelvic floor. If you’re having trouble passing stool, it’s recommended to consult a doctor about treatment options. We recommend beginning with either fiber supplements or dietary changes (the recommended daily allowance for fiber is 25 grams).
Finally
For more information on chronic pain management, pain disorders, chronic pain resources, psychogenic pain, effective chronic pain treatment options, or other physical therapy, you should book a consultation session with a specialist at Chronic Therapy today, give you professional advice that will suit your personal experience.
Also, for people with chronic pain who are constantly worried about how to treat chronic pain or get their chronic pain treated, our specialists of chronic pain symptoms have made huge success over the year in recommending reliable resources to manage chronic pain from nerve pain or any other developing chronic pain conditions.
More to read: Managing Chronic Pain in the Testes




